Scar Revision Surgery: Minimize Scars by Up to 50%
Scar revision surgery offers a significant solution to reduce the visibility of scars from injuries, previous surgeries, or acne, potentially minimizing their appearance by up to 50% through various advanced surgical techniques and subsequent care protocols.
Living with visible scars, whether from an unforeseen injury, a necessary surgical procedure, or persistent acne, can significantly impact one’s confidence and self-perception. For many, these marks are more than just physical reminders; they subtly influence daily interactions and personal comfort. Fortunately, advancements in aesthetic medicine offer tangible solutions for those seeking a smoother skin texture and a more uniform appearance. One such transformative option is scar revision surgery: minimize the appearance of scars from injury, surgery, or acne by up to 50%. This specialized surgical approach isn’t about complete eradication, as no scar can be entirely erased, but rather about enhancing the scar’s aesthetic quality, making it less noticeable and better integrated with the surrounding skin. Through a blend of surgical precision and modern care, individuals can embark on a journey toward renewed confidence, effectively transforming the narrative of their skin’s history.
Understanding the Nature of Scars and Scar Formation
Scars are an inevitable part of the body’s natural healing process following tissue damage. Whether the damage results from an accidental cut, a burn, acne breakouts, or a surgical incision, the body responds by laying down new collagen fibers to repair the wound. This new tissue, however, often differs in texture, color, and thickness from the surrounding skin, leading to the varied appearances of scars we observe. The way a scar forms and its ultimate appearance depend on a multitude of factors, ranging from the depth and size of the wound to its location on the body, an individual’s genetic predisposition, age, and even skin type.
Each scar tells a story of healing, yet some stories are more visibly told than others. Superficial scrapes might leave hardly any trace, blending almost imperceptibly with the skin. Deeper wounds, however, can result in more pronounced scarring. Factors like infection, poor wound healing, or excessive tension on the wound edges during healing can further exacerbate scar formation, leading to scars that are raised, discolored, or otherwise bothersome. Understanding these underlying mechanisms is crucial, as it informs the approach to scar revision, allowing medical professionals to tailor treatments that address the specific characteristics of each scar.
Types of Scars and Their Characteristics
Scars are not monolithic; they manifest in various forms, each with distinct characteristics that dictate the most effective revision strategies. Identifying the type of scar is the first critical step in developing a personalized treatment plan.
- Keloid Scars: These scars are often raised, red or dark, and extend beyond the original wound boundaries. They are typically firm and can be itchy or painful. Keloids are more common in individuals with darker skin tones and tend to recur even after surgical removal.
- Hypertrophic Scars: Similar to keloids, hypertrophic scars are raised and red, but they remain confined to the original wound area. They can also be itchy and may improve over time, though often not completely without intervention.
- Contractures: These scars occur when a large area of skin is lost, often due to burns. The scar tissue pulls the skin and underlying tissue together, leading to a tightening effect that can restrict movement, especially if the scar crosses a joint.
- Acne Scars: These can vary widely, from deep pits (ice pick scars) to rolling or boxcar scars, reflecting the inflammatory and healing processes associated with severe acne breakouts. They often create an uneven skin texture.
- Atrophic Scars: These are sunken scars that form a depression in the skin, often a result of conditions like acne or chickenpox. They occur when the healing process doesn’t generate enough new tissue to fill the wound.
Beyond these primary categories, scars can also present with discoloration, either darker (hyperpigmentation) or lighter (hypopigmentation) than the surrounding skin, adding another layer of complexity to their appearance. The goal of scar revision is not to erase these marks entirely, but to diminish their prominence and improve their texture and color to better blend with the unscarred skin. This comprehensive understanding forms the foundation upon which effective and tailored scar revision strategies are built.
When is Scar Revision Surgery Considered?
The decision to undergo scar revision surgery is deeply personal, often stemming from a desire to improve both physical appearance and emotional well-being. It’s not merely about the scar itself, but about how it impacts an individual’s quality of life. While many scars fade and flatten over time, some remain prominent, disfiguring, or even cause functional impairment, prompting individuals to explore corrective options. The timing and necessity of scar revision are typically determined by a combination of factors, including the scar’s maturity, its impact on daily life, and the patient’s specific goals.
Often, individuals consider scar revision when a scar is causing discomfort, such as itching or pain, or when it restricts movement. Visually, scars that are significantly different in color or texture from the surrounding skin, those that are wide, raised, or depressed, or those that are located in highly visible areas like the face, neck, or hands, frequently lead people to seek revision. Psychological impact also plays a significant role; a prominent scar can lead to self-consciousness, anxiety, or a diminished self-image, making the pursuit of revision a step towards regaining confidence and emotional comfort. Consulting with a board-certified plastic surgeon is crucial to assess the scar’s characteristics and to discuss realistic expectations for improvement.
Evaluating Scar Maturity and Patient Expectations
Scar revision is most effectively performed on mature scars, which typically means waiting at least six to twelve months after the initial injury or surgery. During this period, the scar undergoes a natural maturation process, where its color may lighten, and its texture may soften and flatten. Attempting revision too early can sometimes lead to suboptimal results, as the scar tissue is still actively remodeling. However, in cases where a scar causes severe contracture limiting movement, earlier intervention might be considered. A surgeon will meticulously evaluate the scar’s current state, its type, location, and the patient’s skin characteristics to determine the optimal timing for intervention.
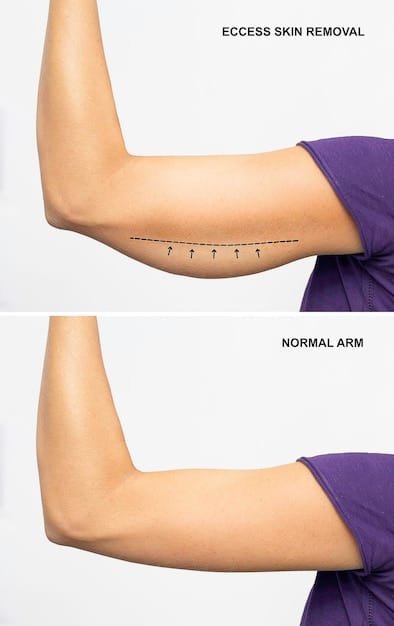
Communicating realistic expectations is paramount in scar revision. It is essential for patients to understand that while revision surgery can significantly improve a scar’s appearance—potentially reducing its visibility by up to 50% or more, depending on the individual case—no scar can be completely eradicated. The goal is to make the scar less noticeable, to improve its texture and color, and to ensure it blends more harmoniously with the surrounding skin. This might involve:
- Making a raised scar flatter and smoother.
- Reducing the width of a wide scar.
- Minimizing the contrast in color between the scar and healthy skin.
- Releasing contractures to restore range of motion.
- Improving the overall contour of the affected area.
The success of scar revision is also heavily influenced by the patient’s immune response, adherence to post-operative care instructions, and individual healing capabilities. A thorough discussion about potential outcomes and the journey ahead ensures that patients are well-informed and emotionally prepared for the process, setting the stage for a satisfying result.

Surgical Techniques for Scar Minimization
Scar revision surgery encompasses a variety of techniques, each carefully selected based on the scar’s specific characteristics, location, and the desired outcome. The overarching goal is to achieve a less conspicuous scar that blends more naturally with the surrounding skin. Modern surgical approaches are sophisticated, combining precision and an understanding of skin dynamics to optimize healing and aesthetic results.
One of the most common surgical techniques is surgical excision, where the old scar is completely removed, and the remaining healthy skin edges are meticulously re-approximated. This may sound straightforward, but the art lies in the careful planning of the new incision line, often oriented to follow natural skin creases or tension lines, making the new scar less noticeable. Advanced wound closure techniques, using fine sutures and minimizing tension, are critical for a superior outcome. For wider or linear scars that are under tension, a technique called Z-plasty or W-plasty might be employed. These methods involve making small, geometric incisions that reorient the scar, breaking up a straight line into a less conspicuous, irregular pattern, which also helps to better distribute skin tension.
Advanced Surgical Approaches and Non-Surgical Adjuncts
Beyond simple excision, surgeons utilize more complex methods for challenging scars. Tissue expansion, for instance, involves inserting a balloon-like expander under healthy skin near the scar. Over several weeks, the expander is gradually filled with saline, stretching the skin. Once enough excess skin has been generated, the expander is removed, and this new, healthy skin can be used to replace the scar tissue. This technique is particularly effective for very large scars where there isn’t enough adjacent skin for direct closure. For contracture scars that restrict movement, Z-plasty is often used to lengthen the scar and release the tension, thereby restoring function.
Surgical scar revision is frequently complemented by non-surgical adjuncts, both before and after the procedure, to enhance the final outcome. These can include:
- Dermabrasion or Laser Resurfacing: These techniques can improve the texture and color of the scar, especially useful for acne scars or scars with irregular surfaces.
- Steroid Injections: For hypertrophic scars and keloids, corticosteroid injections directly into the scar can help flatten and soften the tissue, reducing inflammation and discomfort.
- Topical Treatments: Silicone sheets, gels, and emollients are often recommended post-surgery to aid in scar maturation, reduce redness, and promote a softer texture.
- Pressure Therapy: Applying consistent pressure to a healing scar can help prevent hypertrophy, especially in burn scar management.
- Microneedling: This procedure can stimulate collagen production, improving skin texture and reducing the appearance of atrophic scars.
The combination of these interventions is tailored to each patient, forming a comprehensive plan towards minimizing scar visibility. The collaborative effort between the patient and the surgical team ensures that the most appropriate techniques are employed to achieve the best possible aesthetic and functional outcome, underscoring the personalized nature of scar revision.
The Recovery Process and Post-Operative Care
The journey to minimized scar appearance doesn’t end with the surgery; the recovery process and diligent post-operative care are equally, if not more, crucial for achieving optimal results. How a patient cares for their surgical site in the weeks and months following the procedure significantly influences the final aesthetic outcome. Adherence to surgeon’s instructions, patience, and a proactive approach to wound healing are key components of a successful recovery.
Immediately after scar revision surgery, the treated area will likely be red, swollen, and potentially bruised. Dressings will be applied to protect the wound and support healing. Pain medication may be prescribed to manage any discomfort. It is critical to keep the surgical site clean and dry, change dressings as instructed, and avoid any activities that could put tension on the new incision. Depending on the complexity of the revision, a period of rest and limited activity will be necessary. Factors such as a healthy diet, adequate hydration, and abstaining from smoking can also greatly facilitate the body’s natural healing mechanisms, reducing the risk of complications and promoting a smoother recovery. Regular follow-up appointments with the surgeon are essential to monitor healing progress and address any concerns.
Long-Term Scar Management Strategies
Beyond the initial healing phase, long-term scar management becomes paramount in ensuring the revised scar matures to its best possible appearance. This extended care aims to minimize scar visibility further and prevent potential complications such as hypertrophy or discoloration. The longevity and effectiveness of scar revision often hinge on consistent and diligent adherence to these long-term strategies.
These strategies frequently include:
- Sun Protection: Newly formed scar tissue is highly susceptible to sun damage, which can lead to permanent discoloration (hyperpigmentation). Consistent use of high-SPF sunscreen and protective clothing is vital for at least a year post-surgery.
- Topical Silicone Products: Silicone gels or sheets are widely recommended for their ability to hydrate the scar, reduce collagen overproduction, and improve the scar’s texture and color. They should be applied consistently for several months as per professional guidance.
- Massage Therapy: Gentle massage of the scar site, once cleared by the surgeon, can help break down collagen fibers, soften the scar tissue, and improve its pliability. This can also help reduce itching and discomfort.
- Moisturization: Keeping the scar well-moisturized helps maintain skin elasticity and supports healthy tissue remodeling, preventing dryness and tightness.
- Avoiding Tension: Activities that significantly stretch or pull the skin around the scar should be avoided for several months to prevent widening or elevation of the new scar.
It’s important to remember that scar maturation is a lengthy process, often taking up to 12-18 months. During this time, the scar will continue to evolve, gradually fading and flattening. Patience, coupled with consistent application of these long-term management strategies and ongoing communication with your medical team, will maximize the potential for achieving the best possible aesthetic outcome from scar revision surgery.

Expected Outcomes and Realistic Expectations
Embarking on scar revision surgery means stepping into a process with clear goals and, importantly, a need for realistic expectations. While the promise of minimizing scar appearance by up to 50% is a powerful motivator, it’s crucial to understand that “minimization” does not equate to “erasure.” The objective of scar revision is to improve the scar’s contour, color, and texture so that it becomes less noticeable and blends more seamlessly with the surrounding skin, enhancing both cosmetic appearance and, in some cases, functional ability.
The degree of improvement varies significantly among individuals, influenced by factors such as scar type, location, individual healing capabilities, and adherence to post-operative care. Patients typically observe a softer, flatter, and less discolored scar that is often narrower than the original. For scars causing pain or restricting movement, the revision can lead to a significant improvement in quality of life. Open communication with your plastic surgeon about what to realistically expect is vital to ensure satisfaction with the results. Surgeons will use their expertise to explain the potential outcomes based on your unique circumstances, emphasizing that while the scar will be significantly improved, a faint line or subtle textural difference often remains.
Factors Influencing the Success of Scar Revision
The success of scar revision surgery is not solely dependent on the surgeon’s skill but is a multifactorial process involving the patient’s biological response and their commitment to post-operative guidelines. Several key elements play a pivotal role in determining the final aesthetic and functional outcome.
- Patient’s Age and Health: Younger individuals often have more elastic skin, which can heal well, but also a more active healing response that can sometimes lead to more prominent scarring if not managed carefully. Overall health, including nutritional status and absence of chronic diseases, also impacts healing.
- Scar Characteristics: The type of scar (keloid, hypertrophic, atrophic, etc.), its size, depth, and location profoundly influence achievable outcomes. For instance, keloids have a higher recurrence rate, demanding a more aggressive and combined treatment approach.
- Skin Type and Pigmentation: Individuals with darker skin tones are more prone to hyperpigmentation and keloid formation, requiring tailored surgical techniques and adjunctive therapies.
- Adherence to Post-Operative Care: Diligent follow-through on wound care, sun protection, silicone sheet application, and massage therapy are critical for optimal scar maturation and to prevent complications.
- Surgeon’s Expertise: The experience and skill of a board-certified plastic surgeon are invaluable in selecting the appropriate technique, executing the surgery with precision, and guiding the patient through the recovery process.
Understanding these influences helps set appropriate expectations and encourages active participation from the patient in their recovery journey. While scar revision surgery can bring about remarkable improvements, recognizing its limitations and the ongoing nature of scar maturation empowers patients to appreciate the positive changes the procedure can offer while managing any residual imperfections with a balanced perspective.
Considering the Cost and Insurance Coverage
The decision to undergo scar revision surgery, while often driven by personal comfort and aesthetic desires, naturally involves considerations regarding its financial implications. The cost of scar revision can vary widely, influenced by numerous factors, including the complexity of the procedure, the type of anesthesia used, the geographic location of the practice, and the surgeon’s fees. It’s important for prospective patients to have a clear understanding of these costs and to explore potential insurance coverage options before committing to surgery.
Typically, the total cost for scar revision will encompass the surgeon’s fee, anesthesia fees, and facility charges. Additional expenses might include pre-operative consultations, post-operative medications, and any recommended adjunctive treatments such as steroid injections or laser therapy. Because each scar is unique, a personalized consultation with a plastic surgeon is essential not only to determine the most effective treatment plan but also to receive an accurate estimate of the total cost involved. During this consultation, the surgeon or their office staff should provide a detailed breakdown of all anticipated expenses, allowing the patient to plan accordingly.
Navigating Insurance and Payment Options
When it comes to scar revision surgery, whether insurance will cover the cost is a common and often pivotal question. Generally, cosmetic procedures, which are performed solely to enhance appearance, are not covered by insurance. However, if the scar revision is deemed medically necessary—meaning it addresses a functional impairment or causes significant physical discomfort—a portion or even the entirety of the procedure might be covered. Functional impairments could include scars that restrict movement, cause chronic pain, or lead to psychological distress significant enough to impact daily life.
For patients considering scar revision, it is highly recommended to:
- Consult with Your Surgeon: Discuss with your surgeon if they believe the procedure could be considered medically necessary. They can help provide the necessary documentation and codes for insurance submission.
- Contact Your Insurance Provider: Directly contact your insurance company to understand your policy’s specifics regarding scar revision. Inquire about coverage for cosmetic versus reconstructive procedures, pre-authorization requirements, deductibles, co-pays, and out-of-pocket maximums.
- Obtain Pre-Authorization: If there’s a chance of coverage, your surgeon’s office will typically help with the pre-authorization process, submitting a request to your insurance company with supporting medical documentation.
- Explore Payment Plans: For costs not covered by insurance, many surgical practices offer payment plans or work with third-party financing companies to make the procedure more affordable. Discuss these options during your consultation.
Understanding the financial aspects thoroughly and proactively engaging with both your surgeon’s office and insurance provider can help alleviate stress and ensure that you can focus on the healing process with confidence. This diligent approach ensures that financial considerations do not become an insurmountable barrier to achieving the desired improvements in scar appearance and personal well-being.
Choosing the Right Surgeon for Your Scar Revision
The selection of a qualified and experienced surgeon is arguably the most critical step in ensuring a successful scar revision outcome. This decision goes beyond merely finding a practitioner; it involves identifying a specialist with the precise blend of medical expertise, aesthetic sensibility, and patient-centered communication skills. Given the intricate nature of scar tissue and the varied techniques involved in revision, a surgeon’s proficiency directly impacts the safety and efficacy of the procedure, as well as the ultimate satisfaction of the patient.
A reputable surgeon for scar revision will typically be a board-certified plastic surgeon. Board certification signifies that the surgeon has met rigorous standards of training, experience, and ethical conduct in plastic surgery. This credential provides an assurance of expertise and a commitment to patient safety and quality care. Beyond certification, it is crucial to seek a surgeon with specific experience in scar revision, as this field demands a nuanced understanding of wound healing, skin dynamics, and various surgical and non-surgical modalities. An experienced surgeon will be adept at assessing different scar types, recommending the most appropriate techniques, and managing potential complications, guiding you effectively through the entire process from consultation to post-operative care.
Key Qualifications and Questions to Ask
When evaluating potential surgeons for your scar revision, a thorough vetting process is essential. Beyond board certification, consider the surgeon’s specific experience in scar revision. Look for a surgeon who regularly performs these procedures and demonstrates a deep understanding of the advanced techniques required for optimal results. An artist’s eye for detail and an appreciation for facial and body aesthetics are also invaluable traits, as scar revision is as much an art as it is a science.
During your consultation, be prepared with a list of questions to help inform your decision:
- Board Certification: Is the surgeon board-certified in plastic surgery? Which specific board?
- Experience in Scar Revision: How many scar revision procedures have they performed, and what is their success rate? Can they share before-and-after photos of similar cases?
- Approach to Your Scar: What specific techniques do they recommend for your particular scar, and why? What are the potential risks and benefits of these methods?
- Facility Accreditation: Is the surgical facility accredited? What safety measures are in place?
- Anesthesia Protocol: What type of anesthesia will be used, and who will administer it?
- Costs and Insurance: Provide a detailed breakdown of all costs and discuss insurance coverage possibilities.
- Post-Operative Care Plan: What does the recovery process entail, and what kind of follow-up care will be provided?
- Emergency Protocol: What procedures are in place for managing complications or emergencies?
A surgeon who takes the time to answer these questions thoroughly, explains the procedure in detail, and fosters an environment of trust and open communication is indicative of a professional committed to your well-being. Ultimately, the best surgeon for you will be one with whom you feel comfortable and confident, knowing that your health and aesthetic goals are in capable hands, ensuring a journey towards noticeable scar minimization.
Alternative and Adjunctive Treatments to Consider
While scar revision surgery offers a significant primary solution for minimizing prominent scars, it’s often part of a broader treatment strategy that includes various non-surgical and adjunctive therapies. These complementary treatments can either serve as alternatives for milder scars, enhance the results of surgery, or help manage scars where surgery isn’t the primary option. The holistic approach to scar management aims to improve scar texture, color, and overall appearance, often reducing the need for more invasive procedures or optimizing the outcome of surgical intervention.
For many superficial or newly formed scars, non-surgical options can be remarkably effective. These treatments focus on promoting healthy skin regeneration, reducing inflammation, and evening out skin tone and texture. It’s not uncommon for patients to explore these less invasive routes initially, or to incorporate them into a long-term scar care regimen as recommended by their dermatologist or plastic surgeon. The effectiveness of these treatments can vary based on scar type, patient skin type, and consistency of application or treatment sessions.
A Spectrum of Non-Surgical Scar Management
The landscape of non-surgical scar management is diverse, offering a range of options that can address different scar characteristics. These treatments can be layered or used in sequence to achieve the best possible results.
- Topical Treatments: Silicone gels and sheets are widely regarded for their efficacy in managing hypertrophic and keloid scars. They work by hydrating the scar, regulating collagen production, and reducing itching and discomfort. Onion extract creams and vitamin E are also popular, though scientific evidence for their efficacy is less robust.
- Injections:
- Corticosteroid Injections: Directly injecting steroids into hypertrophic scars or keloids can help flatten them, reduce redness, and alleviate symptoms like itching and pain. Multiple sessions are often required.
- 5-Fluorouracil (5-FU) Injections: This chemotherapy agent, when injected in small doses into scars, can inhibit fibroblast growth and collagen synthesis, proving effective for resistant keloids and hypertrophic scars, often used in conjunction with steroids.
- Laser and Light Therapies:
- Pulsed Dye Lasers (PDL): Effective for red, raised scars (hypertrophic and keloid), PDL targets blood vessels in the scar to reduce redness and flatten the tissue.
- Fractional Lasers (ablative and non-ablative): These lasers create microscopic columns of injury in the skin, stimulating collagen remodeling and improving scar texture, especially for atrophic scars and acne scars.
- Dermabrasion and Microdermabrasion: These mechanical exfoliation techniques remove the top layers of skin, smoothing the surface and improving the appearance of raised or irregular scars, particularly useful for acne scars.
- Chemical Peels: Acid solutions applied to the skin remove outer layers, promoting new skin growth and improving the texture and discoloration of superficial scars.
- Microneedling / Collagen Induction Therapy: Tiny needles create micro-injuries in the skin, stimulating collagen and elastin production, which can significantly improve the appearance of atrophic scars and uneven skin texture.
Choosing the right alternative or adjunctive treatment requires a consultation with a specialist who understands the nuances of scar biology and the capabilities of each therapy. A tailored plan, often combining several approaches, maximizes the potential for scar minimization, helping individuals achieve smoother, more uniform skin with confidence.
| Key Aspect | Brief Description |
|---|---|
| ✨ Scar Minimization | Scar revision surgery can reduce scar appearance by up to 50%, improving texture and color. |
| 🩹 Types of Scars | Vary from keloids and hypertrophic to atrophic and contractures, each requiring specific approaches. |
| 👨⚕️ Surgical Options | Techniques include excision, Z-plasty, W-plasty, and tissue expansion for optimal results. |
| ⏰ Recovery & Care | Post-op adherence, sun protection, and silicone products are vital for scar maturation. |
Frequently Asked Questions About Scar Revision Surgery
A successful scar revision typically means the scar’s appearance is significantly improved, making it less noticeable and blending better with surrounding skin. It often involves reducing its size, flattening its texture, improving its color, and alleviating any discomfort. However, it’s crucial to understand that complete scar removal is unrealistic.
Insurance coverage for scar revision depends on whether it’s deemed medically necessary or purely cosmetic. If the scar causes functional impairment (e.g., restricts movement, causes pain) or significant psychological distress, it may be covered. Cosmetic revisions are generally not covered. Always check with your insurance provider directly.
The surgery duration varies depending on scar complexity but typically ranges from 30 minutes to several hours. Initial recovery involves swelling and bruising for a few weeks. Full scar maturation can take 12-18 months, during which diligent post-operative care, including sun protection and topical treatments, is crucial for optimal results.
There are no strict age restrictions. However, for children, surgeons often recommend waiting until scar tissue has fully matured or the child has reached a certain age to ensure cooperation with post-operative care. For adults, the general health and healing capabilities are more critical factors than chronological age.
Scar revision aims to replace an existing noticeable scar with a less conspicuous one. While the intention is to create a new scar that heals more favorably, it cannot prevent the body’s natural healing process, which always involves scar formation. Optimized surgical techniques and meticulous aftercare help minimize the new scar’s appearance.
Conclusion
Scar revision surgery presents a profound opportunity for individuals to regain confidence and comfort by significantly minimizing the visible impact of scars from injury, past surgeries, or persistent acne. By leveraging advanced surgical techniques, coupled with diligent post-operative care and an array of adjunctive therapies, a reduction in scar appearance of up to 50% or more can often be achieved. This process is a testament to the intricate balance of medical science and personalized care, emphasizing that while scars may be permanent reminders of past events, their narrative on the skin can be thoughtfully rewritten. Choosing an experienced, board-certified plastic surgeon and committing to the comprehensive treatment plan are pivotal steps toward achieving a smoother, more uniform skin appearance, allowing individuals to move forward with renewed self-assurance.





