Bioprinting Breakthroughs: Organs & Tissues for US Healthcare
Bioprinting breakthroughs are transforming US healthcare by enabling the creation of functional organs and tissues, promising to alleviate transplant shortages and usher in an era of personalized regenerative medicine.
The potential of Bioprinting Breakthroughs: Creating Organs and Tissues for US Healthcare represents a paradigm shift in medicine, offering unprecedented solutions to critical health challenges. Imagine a future where organ shortages are a relic of the past, and personalized treatments are the norm. This is the promise that bioprinting holds, a technology rapidly advancing to transform patient care across the United States.
The Dawn of Bioprinting: A New Era in Regenerative Medicine
Bioprinting, at its core, involves the 3D printing of biological materials, such as living cells and biocompatible scaffolds, to create functional tissues and organs. This revolutionary approach aims to overcome the severe limitations of traditional organ transplantation, including donor scarcity, immune rejection, and the need for lifelong immunosuppression. The United States, with its robust research infrastructure and significant investment in biotechnology, is at the forefront of this emerging field.
The journey of bioprinting began with simpler tissue structures, but rapid advancements in bio-inks, printer resolution, and cell biology have propelled it towards more complex applications. Researchers are now capable of creating structures that mimic the intricate architecture and functionality of native human tissues, paving the way for eventual organ fabrication. This scientific endeavor is not merely about replicating form but about ensuring biological function and integration within the human body.
Understanding the Bioprinting Process
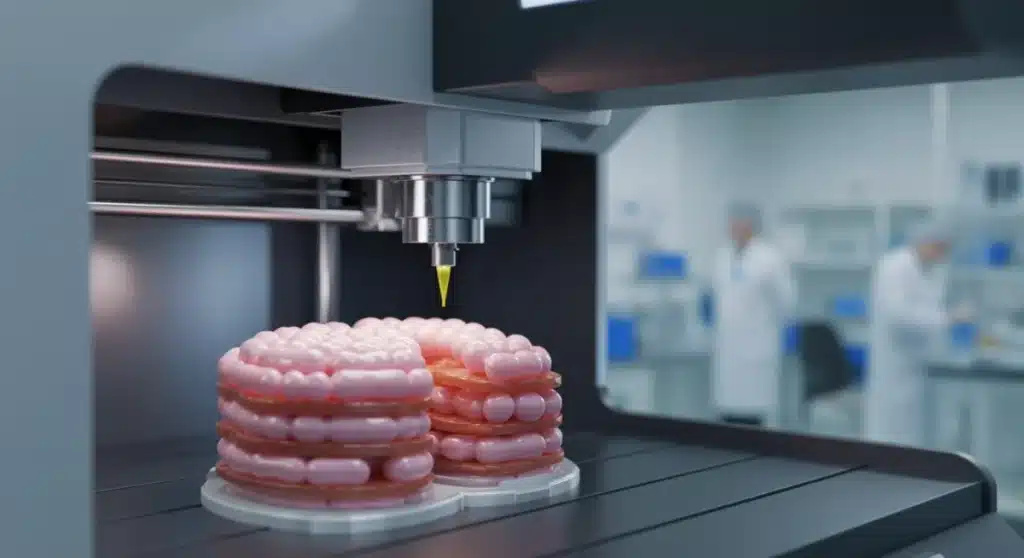
The process of bioprinting typically involves several critical steps, each requiring specialized knowledge and technology. It begins with imaging the target organ or tissue, often using advanced medical scans, to create a precise digital blueprint. This blueprint then guides the bioprinter in layering bio-inks, which are formulations of living cells, growth factors, and biomaterials.
- Bio-ink Development: This involves selecting and formulating materials that support cell viability, proliferation, and differentiation, while also providing structural integrity.
- Printer Technology: Specialized 3D printers are adapted to handle delicate biological materials, ensuring precise deposition and controlled environmental conditions.
- Post-Printing Maturation: Once printed, the construct is often placed in a bioreactor, a device that mimics the physiological environment of the human body, to promote tissue development and functionality.
Each step is crucial for the success of bioprinted constructs, from the initial cellular isolation to the final maturation before potential implantation. The complexity of creating vascularized tissues, essential for nutrient and oxygen delivery, remains a significant challenge but one that researchers are actively addressing with innovative solutions.
The implications of successful bioprinting are profound for US healthcare. It promises not only to reduce the organ donor waiting list but also to revolutionize drug testing, disease modeling, and personalized medicine, offering tailor-made solutions for individual patients based on their unique genetic and physiological profiles. This shift represents a move from generalized treatments to highly specific, patient-centric interventions.
Addressing the Organ Shortage Crisis with Bioprinting
The organ shortage crisis in the United States is dire, with thousands of patients dying each year while awaiting a life-saving transplant. The demand for organs far outstrips the available supply, creating an urgent need for alternative solutions. Bioprinting emerges as a beacon of hope in this challenging landscape, offering the potential to create organs on demand, specific to a patient’s needs, thereby circumventing the ethical and logistical hurdles of traditional organ donation.
Current statistics highlight the severity of the problem: over 100,000 Americans are on the national transplant waiting list, and a new person is added every 9 minutes. While living and deceased donors contribute significantly, their numbers are insufficient to meet the overwhelming demand. Bioprinting could fundamentally alter these numbers, offering a sustainable source of functional organs.
The Promise of Patient-Specific Organs
One of the most compelling aspects of bioprinting is the ability to create patient-specific organs using the patient’s own cells. This significantly reduces the risk of immune rejection, a major complication in conventional transplantation that necessitates lifelong immunosuppressive therapy with its associated side effects. By eliminating or minimizing immune suppression, bioprinting promises a higher quality of life for transplant recipients.
Imagine a future where a patient with kidney failure doesn’t wait for a donor, but instead has a new, functional kidney bioprinted from their own cells. This personalized approach extends beyond simple organ replacement; it opens doors for repairing damaged tissues within existing organs, offering restorative rather than just replacement therapies. The precision of bioprinting allows for customization in size, shape, and cellular composition, perfectly matching the recipient’s anatomy.
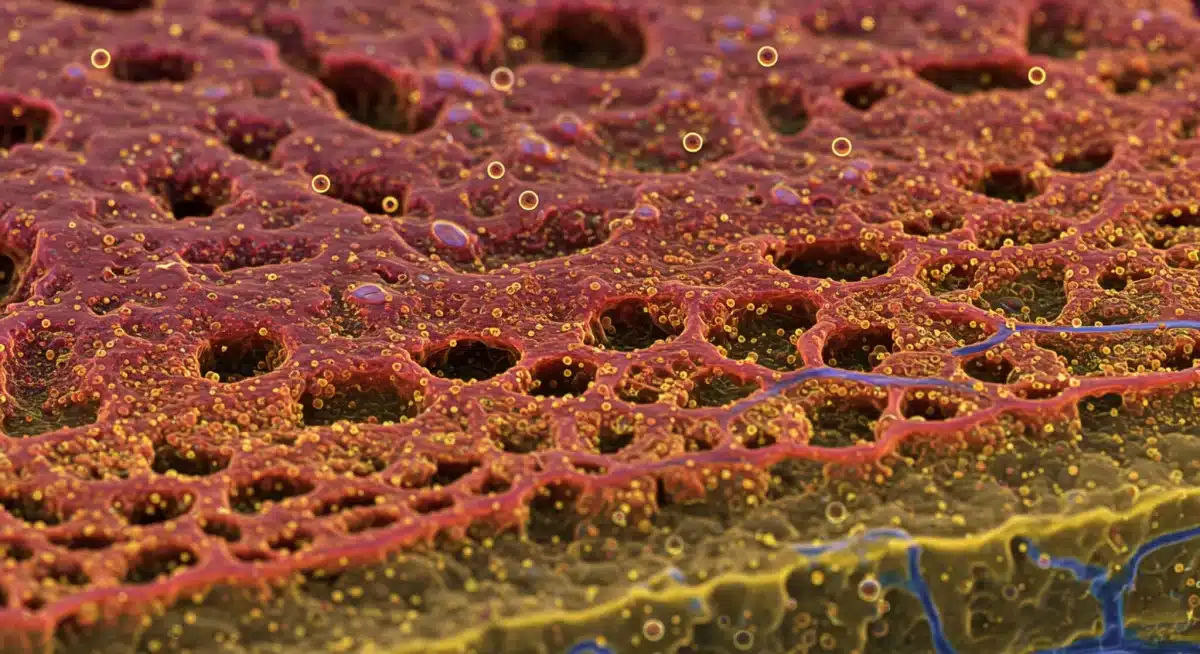
The development of vascular networks within bioprinted organs is a critical area of research. Without a functional blood supply, larger bioprinted tissues cannot survive. Scientists are employing advanced techniques, such as incorporating endothelial cells and designing intricate microfluidic channels, to ensure adequate oxygen and nutrient delivery, mimicking natural vascularization. These efforts are bringing the vision of fully functional bioprinted organs closer to reality.
While still in its early stages for complex organs, bioprinting has already demonstrated success in creating simpler tissues like skin grafts and cartilage. These early successes provide a crucial proof-of-concept and a roadmap for tackling more complex structures, gradually moving towards the ultimate goal of printing entire human organs for transplantation. The impact on US healthcare, particularly for chronic diseases requiring organ replacement, would be transformative.
Technological Advancements Driving Bioprinting Innovation
The rapid progression of bioprinting is largely attributable to significant technological advancements across multiple disciplines. From materials science to computer-aided design, each area contributes to the sophistication and feasibility of creating complex biological structures. These innovations are not just incremental improvements but represent fundamental shifts in capabilities.
One of the most critical areas of advancement is in the development of novel bio-inks. Early bio-inks were limited in their ability to support cell viability and provide adequate structural support. Today, researchers are engineering advanced hydrogels and other biomaterials that can precisely mimic the extracellular matrix of native tissues, providing the ideal environment for cell growth and differentiation. These new bio-inks are often smart materials, responding to various stimuli to facilitate tissue maturation.
Precision and Resolution in 3D Bioprinters
The printers themselves have undergone substantial improvements. Modern bioprinters offer unprecedented levels of precision and resolution, capable of depositing cells and biomaterials with micron-level accuracy. This fine control is essential for replicating the intricate microarchitecture of human tissues, which is vital for their proper function. Different bioprinting techniques have emerged, each with its own advantages:
- Extrusion-based bioprinting: Offers high cell viability and material versatility, suitable for larger constructs.
- Inkjet-based bioprinting: Provides high resolution and speed, ideal for patterning cells in thin layers.
- Laser-assisted bioprinting: Excels in high-resolution printing of complex geometries, though often with higher costs.
The convergence of these technologies allows researchers to select the most appropriate method for specific tissue engineering challenges, optimizing for cell viability, resolution, and scalability. The ability to combine multiple printing modalities within a single system further expands the possibilities, enabling the creation of multi-material and multi-cellular constructs.
Computational modeling and artificial intelligence (AI) are also playing increasingly vital roles. AI algorithms can analyze vast datasets of biological information to design optimal tissue structures and predict cell behavior within printed constructs. This accelerates the research and development cycle, allowing for more efficient experimentation and refinement of bioprinting protocols. The integration of AI not only streamlines the design process but also enhances the functional outcome of bioprinted tissues.
These technological strides are collectively pushing the boundaries of what is possible in bioprinting, moving it from theoretical concept to tangible solutions for medical challenges. The continuous innovation in materials, hardware, and computational tools ensures that bioprinting will remain a dynamic and rapidly evolving field, poised to make significant contributions to healthcare in the US and globally.
Ethical Considerations and Regulatory Pathways in Bioprinting
As with any groundbreaking medical technology, bioprinting raises a complex array of ethical considerations and necessitates clear regulatory pathways. The ability to create human tissues and organs from scratch brings forth questions about the definition of life, the commercialization of body parts, and equitable access to these advanced therapies. Navigating these ethical landscapes is crucial for the responsible development and implementation of bioprinting in US healthcare.
One primary ethical concern revolves around the source of cells used for bioprinting, particularly when human embryonic stem cells or induced pluripotent stem cells are involved. While these cells offer immense potential due to their plasticity, their use often sparks debate. Researchers are actively exploring adult stem cells and other somatic cell sources to mitigate some of these concerns, striving for solutions that are both scientifically effective and ethically sound.
Navigating Regulatory Frameworks for Bioprinted Products
The regulatory pathway for bioprinted organs and tissues is still evolving, posing significant challenges for researchers and developers. In the US, the Food and Drug Administration (FDA) is responsible for overseeing these advanced therapies, which often fall under the category of biologics or medical devices, or a combination of both. The unique nature of living constructs requires a tailored regulatory approach that addresses both safety and efficacy.
- Safety Assessment: Ensuring that bioprinted products are free from contamination, do not elicit adverse immune responses, and behave predictably within the body.
- Efficacy Evaluation: Verifying that the bioprinted tissue or organ performs its intended physiological function effectively and durably.
- Long-term Monitoring: Establishing protocols for post-market surveillance to track the performance and safety of these products over extended periods.
The FDA has been proactive in engaging with the bioprinting community, issuing guidance documents and holding workshops to clarify expectations and facilitate innovation while ensuring patient safety. This collaborative approach is essential for establishing a robust and predictable regulatory environment that supports responsible development without stifling progress. The journey from laboratory bench to clinical application is lengthy and arduous, particularly for novel technologies like bioprinting.
Moreover, equitable access to bioprinted organs and tissues is a significant ethical consideration. As these therapies are likely to be expensive initially, there is a risk that they could exacerbate existing healthcare disparities. Policymakers and healthcare systems must proactively address how these life-saving technologies can be made accessible to all who need them, regardless of socioeconomic status. This involves discussions about pricing, insurance coverage, and public funding for research and development.
Addressing these ethical and regulatory challenges is paramount for bioprinting to realize its full potential in revolutionizing US healthcare. A thoughtful and collaborative approach, involving scientists, ethicists, regulators, and policymakers, will be necessary to ensure that these breakthroughs benefit society broadly and responsibly.
Impact on Personalized Medicine and Drug Discovery
Beyond organ replacement, bioprinting is poised to have a transformative impact on personalized medicine and drug discovery. The ability to create functional, patient-specific tissues outside the body provides an unprecedented platform for understanding disease mechanisms, testing new therapies, and tailoring treatments to individual genetic profiles. This shift promises to make healthcare more precise, effective, and efficient.
In personalized medicine, bioprinted tissues derived from a patient’s own cells can serve as highly accurate models for disease. For instance, a patient with a rare genetic disorder affecting cardiac function could have miniature heart tissue bioprinted from their cells. This ‘heart-on-a-chip’ could then be used to observe disease progression, test the efficacy of different drugs, and identify the most suitable treatment regimen without exposing the patient to potentially harmful experimental therapies.
Revolutionizing Drug Testing and Development
The traditional drug discovery process is notoriously long, expensive, and often yields high failure rates, partly due to the limitations of animal models and two-dimensional cell cultures. Bioprinted 3D tissue models offer a more physiologically relevant alternative, better mimicking the complex environment and cellular interactions found in living human organs. This can significantly improve the accuracy of drug screening and reduce the need for animal testing.
- Reduced Animal Testing: Bioprinted human tissues can replace some animal models, addressing ethical concerns and often yielding more relevant data.
- Enhanced Drug Efficacy Prediction: 3D tissue models can more accurately predict how a drug will behave in the human body, leading to fewer failures in clinical trials.
- Accelerated Drug Development: More efficient screening processes can shorten the timeline from drug discovery to market, bringing new treatments to patients faster.
Pharmaceutical companies are increasingly investing in bioprinting technologies to create ‘organoids’ or ‘organs-on-chips’ that can simulate various human organs, including the liver, kidney, and brain. These micro-physiological systems allow for comprehensive studies of drug metabolism, toxicity, and efficacy in a controlled, human-specific environment. This is particularly valuable for developing drugs for complex diseases where animal models have proven inadequate.
The integration of bioprinting into drug discovery also facilitates the identification of patient-specific biomarkers and drug responses. By testing drugs on bioprinted tissues derived from diverse patient populations, researchers can better understand why certain individuals respond differently to medications, paving the way for truly personalized pharmacotherapy. This level of precision can lead to safer and more effective treatments, minimizing adverse reactions and maximizing therapeutic benefits.
Ultimately, bioprinting’s contributions to personalized medicine and drug discovery will reshape how diseases are understood, treated, and prevented. It represents a fundamental shift towards a more predictive, preventive, personalized, and participatory healthcare model, significantly benefiting patients across the US by offering tailored and highly effective medical interventions.
Challenges and Future Directions for Bioprinting in US Healthcare
Despite the remarkable progress, bioprinting still faces significant challenges before fully integrating into mainstream US healthcare. Overcoming these hurdles will require continued innovation, substantial investment, and collaborative efforts across scientific, medical, and policy sectors. The path from laboratory success to clinical reality is complex and multi-faceted.
One of the most formidable challenges lies in scaling up the production of bioprinted organs and tissues. While printing small tissue constructs is achievable, creating a full-sized, vascularized organ with the necessary cellular complexity and functional longevity remains an engineering marvel yet to be perfected. The sheer number of cells required for a human organ, coupled with the need for precise vascularization to ensure cell survival, presents a massive technical barrier. Researchers are exploring advanced techniques, such as perfusable hydrogels and integrating existing vascular networks, to address this.
Ensuring Long-Term Viability and Functionality
Another critical area of focus is ensuring the long-term viability and functionality of bioprinted constructs once implanted. Unlike synthetic implants, bioprinted tissues are living entities that must integrate seamlessly with the host’s body, grow, adapt, and maintain function over many years. This requires a deep understanding of tissue maturation, remodeling, and interaction with the host immune system.
- Vascularization: Developing robust blood vessel networks within bioprinted organs to supply nutrients and remove waste, crucial for long-term survival.
- Innervation: Integrating nerve cells to allow for proper sensory and motor function, particularly important for complex organs.
- Immune Integration: Ensuring that bioprinted tissues are not rejected by the host’s immune system, even when using patient-specific cells.
The cost of bioprinting technology and personalized treatments is also a major challenge. The research and development, specialized equipment, and highly skilled personnel required make these therapies potentially very expensive. Developing cost-effective methods for cell sourcing, bio-ink production, and printing will be essential for widespread adoption and equitable access within the US healthcare system.
Looking ahead, the future of bioprinting in US healthcare is characterized by continued interdisciplinary collaboration. Biomedical engineers, cell biologists, clinicians, materials scientists, and ethicists must work together to push the boundaries of what is possible. Investment in advanced research infrastructure, funding for translational studies, and streamlined regulatory processes will be vital to accelerate the transition of bioprinting from experimental science to clinical practice.
The ultimate goal is not just to replace organs but to restore health and improve the quality of life for millions. Bioprinting, with its promise of on-demand, personalized organs and tissues, represents one of the most exciting and impactful frontiers in modern medicine, holding the potential to redefine healthcare as we know it in the coming decades.
Bioprinting in Clinical Trials: Early Successes and Hopes
While the vision of bioprinted full organs for transplantation is still a future endeavor, bioprinting technology is already making inroads into clinical trials and showing promising early successes for simpler tissue structures. These initial clinical applications provide invaluable data, refine methodologies, and build confidence in the safety and efficacy of bioprinted products. The US healthcare system is actively supporting these pioneering efforts, understanding their foundational importance.
One of the most notable areas of early clinical application is in skin tissue engineering. Patients with severe burns or chronic wounds often face limited treatment options, and traditional skin grafts can be painful and scarce. Bioprinted skin, created from a patient’s own cells, offers a potential solution by providing a custom-fit, functional skin substitute that promotes healing and reduces scarring. Several research groups and companies in the US are developing bioprinted skin models for clinical use, with some already entering early-phase human trials.
Advancements in Cartilage and Bone Repair
Another area seeing significant progress in clinical trials is the bioprinting of cartilage and bone tissues for orthopedic applications. Joint injuries, osteoarthritis, and bone defects are common conditions that often require surgical intervention and can lead to long-term disability. Bioprinted cartilage and bone scaffolds, seeded with patient-derived cells, aim to regenerate damaged tissue rather than merely repairing it, offering more durable and natural outcomes.
- Cartilage Regeneration: Bioprinted cartilage constructs are being tested for repairing articular cartilage defects in knees and other joints, aiming to restore smooth joint function.
- Bone Graft Alternatives: Customized bioprinted bone scaffolds are explored as alternatives to traditional bone grafts, especially for complex or large bone defects.
- Spinal Fusion: Bioprinted constructs are under investigation for enhancing spinal fusion procedures, providing stable and biologically active support.
These early clinical trials, while often small and focused on safety, are crucial for demonstrating the feasibility and potential benefits of bioprinting. They help identify unforeseen challenges, optimize surgical techniques for implantation, and gather critical data on patient outcomes. The iterative nature of these trials ensures that the technology is refined and made safer before broader application.
Beyond direct implantation, bioprinting is also being explored for creating advanced wound dressings and drug delivery systems. For instance, bioprinted patches can be designed to release growth factors or antibiotics directly to a wound site, promoting faster and more effective healing. These applications, though less complex than full organ printing, represent important steps in integrating bioprinting into everyday clinical practice.
The successes from these clinical trials provide significant hope and motivation for the broader field of bioprinting. Each positive outcome brings the US healthcare system closer to a future where regenerative therapies, powered by bioprinting, are a standard part of patient care, significantly improving lives and transforming treatment paradigms for a wide range of conditions.
Economic Implications and Investment in Bioprinting
The economic implications of bioprinting breakthroughs for US healthcare are substantial, encompassing market growth, investment opportunities, and potential cost savings in the long run. As the technology matures and moves closer to clinical application, it is attracting significant capital and fostering a new segment within the biotechnology industry. Understanding these economic dynamics is key to appreciating the full impact of bioprinting.
The global market for 3D bioprinting is projected to experience exponential growth in the coming years, with the US being a major driver of this expansion. This growth is fueled by increasing demand for organ transplantation, the need for better drug testing models, and advancements in personalized medicine. Investment is flowing from various sources, including venture capital firms, pharmaceutical companies, and government grants, recognizing the immense potential for both medical breakthroughs and financial returns.
Investment Landscape and Market Projections
The investment landscape for bioprinting is dynamic, with a focus on companies developing advanced bioprinters, novel bio-inks, and specialized tissue engineering services. Startups are emerging with innovative solutions, while established medical device manufacturers and biotech giants are acquiring or partnering with these smaller entities to integrate bioprinting capabilities into their portfolios. This consolidation and collaboration are accelerating the pace of development.
- Venture Capital: Significant funding rounds for bioprinting startups, indicating strong investor confidence in future profitability.
- Government Funding: Grants from agencies like the National Institutes of Health (NIH) supporting fundamental research and translational studies in bioprinting.
- Pharmaceutical Partnerships: Collaborations between bioprinting companies and pharma giants to develop advanced drug screening platforms.
While the initial costs of developing and implementing bioprinting technologies are high, the long-term economic benefits could be immense. By reducing the need for costly immunosuppressive drugs, shortening hospital stays, and improving patient outcomes, bioprinted organs and tissues could lead to significant savings for the healthcare system. Furthermore, the ability to conduct more accurate drug discovery could drastically cut development costs and bring more effective treatments to market faster.
The creation of bioprinted organs on demand could also alleviate the economic burden associated with chronic organ failure, which often involves extensive dialysis, complex surgical procedures, and lifelong medical management. A successful bioprinted organ could offer a one-time, curative solution, fundamentally changing the cost-benefit analysis of organ replacement therapies.
Moreover, the bioprinting industry is creating new jobs and fostering a highly skilled workforce in engineering, biology, and medicine. This economic activity contributes to national prosperity and reinforces the US’s position as a global leader in medical innovation. The economic impact of bioprinting extends beyond direct healthcare costs, influencing research, manufacturing, and education sectors across the country, making it a critical area for continued investment and strategic development.
| Key Aspect | Brief Description |
|---|---|
| Organ Shortage Solution | Bioprinting offers a promising solution to the critical lack of donor organs, potentially creating patient-specific tissues and organs on demand. |
| Personalized Medicine | Enables the creation of patient-specific tissues from their own cells, reducing immune rejection and tailoring treatments for individual needs. |
| Drug Discovery Impact | Provides more accurate 3D human tissue models for drug testing, reducing reliance on animal models and accelerating drug development. |
| Ethical & Regulatory | Requires careful navigation of ethical concerns and evolving FDA regulations to ensure safe and equitable access to these advanced therapies. |
Frequently Asked Questions About Bioprinting
Bioprinting is a 3D printing technology that uses biological materials, such as living cells and biocompatible scaffolds (bio-inks), to create functional tissues and organs. It aims to replicate natural biological structures for medical applications like transplantation and drug testing.
Bioprinting holds the potential to create organs on demand using a patient’s own cells, thereby circumventing the scarcity of donor organs and reducing the risk of immune rejection. This could significantly shorten transplant waiting lists.
Key challenges include scaling up production, achieving adequate vascularization (blood supply) within larger constructs, ensuring long-term viability and functionality, and navigating complex regulatory and ethical landscapes.
It will allow for the creation of patient-specific disease models and drug testing platforms, improving the accuracy of drug screening, reducing animal testing, and enabling tailored treatments based on individual genetic profiles.
While simpler tissues like skin and cartilage are in early clinical trials, complex organs are still decades away from widespread clinical availability. Significant research and regulatory hurdles must be overcome first.
Conclusion
The journey of bioprinting, from its earliest experiments to the current Bioprinting Breakthroughs: Creating Organs and Tissues for US Healthcare, highlights the extraordinary capacity of science to push boundaries once thought impossible.
What was once theoretical is now edging closer to clinical reality, with researchers printing blood vessels, skin, and even complex organ structures that could redefine the future of medicine.
Yet, this path is not without obstacles. The creation of fully functional organs requires solving challenges in vascularization, scalability, and long-term biocompatibility.
Still, advances such as the recent development of 3D-printed blood vessels show how rapidly the field is progressing, offering a glimpse of how close we may be to viable transplant-ready solutions.
These milestones illustrate not only scientific progress but also the potential to address the critical organ shortage crisis in the U.S.
Looking ahead, the promise of bioprinting lies in its ability to merge personalized medicine, regenerative therapies, and innovative technologies into solutions that could transform patient care.
With continued investment, cross-disciplinary collaboration, and careful attention to ethical frameworks, the field is poised to revolutionize healthcare.
Bioprinting may soon shift from experimental innovation to everyday medical practice, providing hope and life-saving opportunities for millions of patients.





